Facing the challenges of securing benefits can be tough. Many veterans deal with service-connected conditions impacting their lives. VA Disability for Eating Disorders is one of these challenges.
If you’re a veteran with an eating disorder, it might surprise you how common this is. Did you know that 9% of male veterans and 19% of women veterans experience eating disorders? You are not alone in dealing with this issue and securing VA Disability for Eating Disorders potentially stemming from your service.
Understanding Eating Disorders in the Context of Military Service
Military service can have various stressors that increase the risk of eating disorders. These may show up during active duty or even after service ends.
It can take time for veterans to adjust when returning to civilian life. This transition can be a significant factor.
Research shows a link between trauma and disordered eating behaviors. A 2017 VA-funded study found this connection, proving it’s more than coincidence.
What Counts as an Eating Disorder for VA Disability?
The VA recognizes specific eating disorders under its rating schedule. The VA considers anorexia nervosa (Diagnostic Code 9520) and bulimia nervosa (Diagnostic Code 9521). However, the criteria used for these can apply to other eating disorders.
Conditions like binge eating disorder fall under the same guidelines. The core issue is persistent eating behaviors related to food and body image that negatively impact health. These behaviors could disrupt daily life.
Consider individuals with obsessive and/or constant thoughts about weight, shape, and food. This leads to unhealthy eating patterns, often more severe than realized.
Common Types of Eating Disorders Among Veterans
Several eating disorders commonly affect veterans. Each has its own impacts on a person’s well-being.
Anorexia Nervosa involves a strong fear of weight gain. There are usually behaviors to restrict calorie intake to prevent weight gain.
Bulimia Nervosa has cycles of binge eating, where large amounts of food are consumed quickly. These behaviors can be hidden without consistent communication.
Binge Eating Disorder: A Growing Concern
Binge Eating Disorder (BED) is common and requires attention. It has frequent episodes of eating large amounts of food, often quickly and to the point of discomfort.
This isn’t occasional overeating. A key part of BED is feeling unable to stop or control eating, leading to shame.
Many with BED don’t use compensatory behaviors. Frequent binge eating can cause medical issues.
Establishing Service Connection for Eating Disorders
Getting VA disability benefits for an eating disorder requires showing “service connection.” You must demonstrate a link between your service and the condition.
This involves three key elements. First, a current diagnosis from a doctor for your eating disorders. Second, you experienced something during your military career, evident in VA records. Third, a doctor confirms the connection.
A clear diagnosis of anorexia nervosa or bulimia nervosa is crucial. But a diagnosis isn’t sufficient. You’ll need evidence of why it developed during service.

Direct Service Connection Explained
Direct service connection means your eating disorder began during active service. Events or stressors of military life directly led to the condition.
Documented events or medical records are essential evidence. A medical professional must support your claim, establishing an in-service event. This is what you believe triggered the condition.
Consider military sexual trauma (MST), which has lower evidence requirements. Intense physical demands, traumatic events, or training can also be factors.
Secondary Service Connection: When Other Conditions Contribute
Sometimes, an eating disorder develops due to another service-connected condition, like Post-Traumatic Stress Disorder (PTSD).
If your service-connected PTSD contributed to your eating disorders, you could claim it as a secondary condition. Proving this requires medical evidence. The evidence must confirm that your eating disorder resulted from your service-connected PTSD.
For example, intense emotional distress might lead to using food for control. This can result in disordered eating patterns.
VA’s Rating System for Eating Disorders
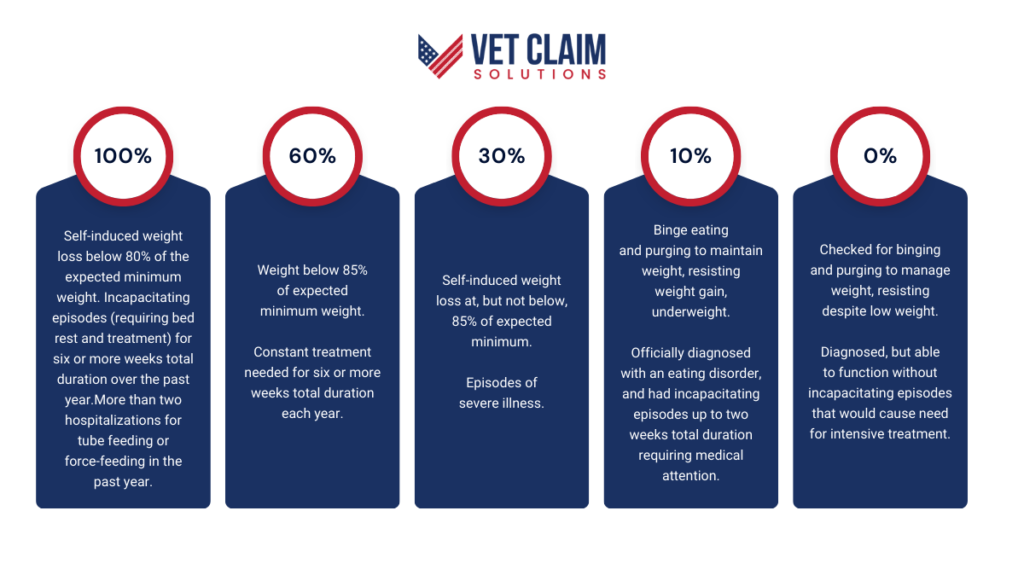
Once service connection is approved, the VA assigns a disability rating. The VA uses criteria in 38 CFR § 4.130. VA ratings depend on the condition’s severity, its impact on life, and treatment needs.
The VA uses a scale: 0%, 10%, 30%, 60%, or 100%. This percentage guides payments, benefits, and services. Key factors, like “incapacitating episodes,” are considered.
These refer to how severe the condition becomes, requiring bed rest. A licensed health professional determines this.
Understanding the Rating Percentages
Let’s examine how the VA measures severity. These guidelines depend on factors from your minimum weight to constant care needs.
| Disability Rating | Criteria |
| 100% | Self-induced weight loss below 80% of the expected minimum weight.Incapacitating episodes (requiring bed rest and treatment) for six or more weeks total duration over the past year.More than two hospitalizations for tube feeding or force-feeding in the past year. |
| 60% | Weight below 85% of expected minimum weight.Constant treatment needed for six or more weeks total duration each year. |
| 30% | Self-induced weight loss at, but not below, 85% of expected minimum.Episodes of severe illness. |
| 10% | Binge eating and purging to maintain weight, resisting weight gain.Underweight.Officially diagnosed with an eating disorder, and had incapacitating episodes up to two weeks total duration requiring medical attention. |
| 0% | Checked for binging and purging to manage weight, resisting despite low weight.Diagnosed, but able to function without incapacitating episodes that would cause need for intensive treatment. |
What “Incapacitating Episode” Means
The term “incapacitating episode” is important in VA disability claims for eating disorders. It means professional care, including rest and bed rest, is necessary.
It’s more than just a bad day. It involves needing time off and following a physician’s orders.
Gathering Evidence and Building Your Claim
Collecting all evidence and documentation for a solid VA claim is important. A denial doesn’t mean it is over.
Gather medical diagnoses, treatment records, and evidence linking your condition to service. Doctors should provide a nexus letter and supporting evidence. This isn’t about going it alone.
Strong cases are built step-by-step. Organize all your evidence to present a clear case.
Medical Records: Your Primary Evidence
VA disability claims require medical evidence for assessment. This isn’t to question the eating disorder, but to assess your current medical status.
Current and complete medical documents allow the VA to determine if a VA disability rating warrants payment. Include hospital stays or tube feeding information. Don’t exclude outpatient care or discussions with doctors.
It highlights challenges faced by those providing care. Even minor symptoms could support a service connection.

Getting a Diagnosis: Don’t Delay
You need an evaluation by a medical professional who can diagnose your condition. Don’t delay. Getting started can lead to prompt treatment. Ignoring the issue could result in lasting problems.
This can involve tests like blood counts. It can also include checks for heart issues. The VA needs to know your current condition, and this assessment is vital.
It might give veterans opportunities to increase an eating disorder VA rating from their service.
Beyond Medical Records: Other Supporting Documents
Personal stories, statements from friends or family, and service records. These can provide a comprehensive view.
Sometimes, the connection is obvious. You may recall an event that changed everything.
Other times, additional support can help you identify the root causes. Did others witness a significant incident?
Lay Statements: A Personal Perspective
Lay statements from veterans or loved ones offer another perspective. These can add details you might overlook. What you consider trivial, your support network might not.
Recall a moment you confided in someone during active duty. Describe it. Did your buddy observe a difficult period?
Your spouse noticing behavioral changes is powerful. Were they the ones who urged you to seek help? Did they express concerns that others dismissed? Friends or comrades sharing observed patterns are also crucial.
What Happens After You Submit Your Claim?
The VA determines if the condition is linked to your deployment or reserve activation. They consider the full impact to decide on support, including services, disability payments, or other aid.
They might require a Compensation & Pension (C&P) exam. You must gather support before a denial.
They review medical records and evidence. Include records from treatment professionals. Lay statements from close contacts can be valuable.
Possible Outcomes: Denial, Approval, or a Different Rating
The review may result in the VA approving your claim, leading to benefits. This is good news. The VA may also deny the connection, feeling it’s not service-related. Or, it might assign a lower VA rating than your medical records indicate, which is important to know.
If you receive an unexpected outcome, be aware of next steps. There might be ways to improve an existing or past result if details were initially missed.
Denial options include a supplemental claim, higher-level review. Persistence matters, even if the initial outcome is frustrating. If you need to file or face issues, Vet Claim Solutions can help.
Resources and Support for Veterans with Eating Disorders
Dealing with eating issues can feel isolating. There’s no need to go through it alone.
Veterans facing these conditions can benefit from available resources. Finding ways to manage challenges and achieve lasting improvements.
Support includes groups sharing experiences, professionals offering tools, and 24/7 crisis support. Consider VA options and facilities with trained professionals.
The Veteran Crisis Line is always available, anytime, day or night. Don’t hesitate to reach out for immediate support.
Consider these additional resources:
- ANAD Helpline: 1 (888) 375-7767, Monday-Friday, 9am-9pm CT.
- National Alliance for Eating Disorders Helpline: 1 (866) 662-1235, Monday-Friday, 9am-7pm ET.
Conclusion
Securing VA Disability for Eating Disorders involves more than just following procedures. Veterans need to know they can address concerns stemming from their service.
Gathering military records, medical evaluations, and personal statements is important. You might need help with your disability claim, which we can provide.
Understanding benefits, navigating requirements, and finding treatment becomes easier with action. While the process may have challenges, accurate claims improve your chances. With Vet Claim Solutions, you receive guidance from an experienced team.


