Heard whispers about VA sleep apnea ratings changing? You’re not alone. Many veterans worry about what these potential updates might mean for their disability benefits. Fully understanding upcoming changes in VA sleep apnea rating criteria helps you prepare for what might come.
But here’s the thing: nothing is set in stone yet. This uncertainty makes understanding upcoming changes in VA sleep apnea rating criteria feel confusing; we get it.
This blog post breaks down what we know, what’s still up in the air, and why acting now could be very important for your VA disability claim. We hope you enjoy reading and find this information helpful.
What Exactly is Sleep Apnea?
Sleep apnea isn’t just loud snoring; it’s a serious sleep disorder. It’s characterized by breathing that repeatedly stops and starts during sleep. These pauses can last for several seconds or even longer.
These interruptions might occur 30 times or more within an hour. There are three main types recognized by medical professionals. Obstructive sleep apnea (OSA) is the most frequent type, resulting from the throat muscles relaxing excessively during sleep.
Central sleep apnea (CSA) occurs when the brain fails to send the correct signals to the muscles controlling breathing. Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, involves having both OSA and CSA. Identifying the specific type is crucial for effective treatment.
Common sleep apnea symptoms include loud snoring, gasping for air during sleep, morning headaches, and excessive daytime sleepiness. Difficulty concentrating and irritability are also frequently reported apnea symptoms. Ignoring these signs can lead to significant health consequences.
Left untreated, sleep apnea can contribute to serious health conditions. These include high blood pressure, heart problems like heart attacks and strokes, type 2 diabetes, and liver problems. The constant disruption of sleep also leads to persistent daytime fatigue and difficulty concentrating.
Getting a proper diagnosis is the first step towards management. This typically involves an overnight sleep study, known as a polysomnogram, often detailed by sources like the National Heart, Lung, and Blood Institute. This study monitors brain waves, heart rate, breathing patterns, and blood oxygen levels during sleep.

Sleep Apnea’s Connection to Military Service
Why does sleep apnea seem particularly prevalent among veterans? Several factors related to military life can increase the risk or worsen sleep apnea. Exposure to environmental hazards like burn pits, dust, and fumes during deployment is one significant area under investigation.
Certain health conditions frequently linked to military service also show a strong correlation with sleep apnea. Conditions like post-traumatic stress disorder (PTSD), a common mental health issue among veterans, are closely associated. Research consistently indicates that veterans diagnosed with PTSD have a considerably higher risk of developing OSA.
The physical demands and stresses of service can also contribute. Weight gain, often a consequence of service-connected injuries limiting mobility or associated with certain mental health conditions, is a major risk factor for OSA. Injuries themselves, such as a Traumatic Brain Injury (TBI), might also be biologically linked to the development of sleep apnea.
Furthermore, other common service-related conditions like chronic sinusitis or rhinitis can obstruct airways and potentially lead to or worsen sleep apnea. Even exposure to loud noises impacting sleep patterns might play a role. Essentially, various facets of military life can initiate or exacerbate this breathing disorder, making it a common disability claim for veterans.
How the VA Rates Sleep Apnea Right Now
Currently, the VA evaluates sleep apnea under 38 CFR § 4.97, Diagnostic Code 6847. The assigned disability rating percentage depends primarily on the necessary treatment and the severity of symptoms experienced by the veteran.
The current rating criteria based system is relatively direct. Your VA disability rating is largely determined by the level of medical intervention required to manage the condition.
Here’s a simplified breakdown of the current sleep apnea ratings:
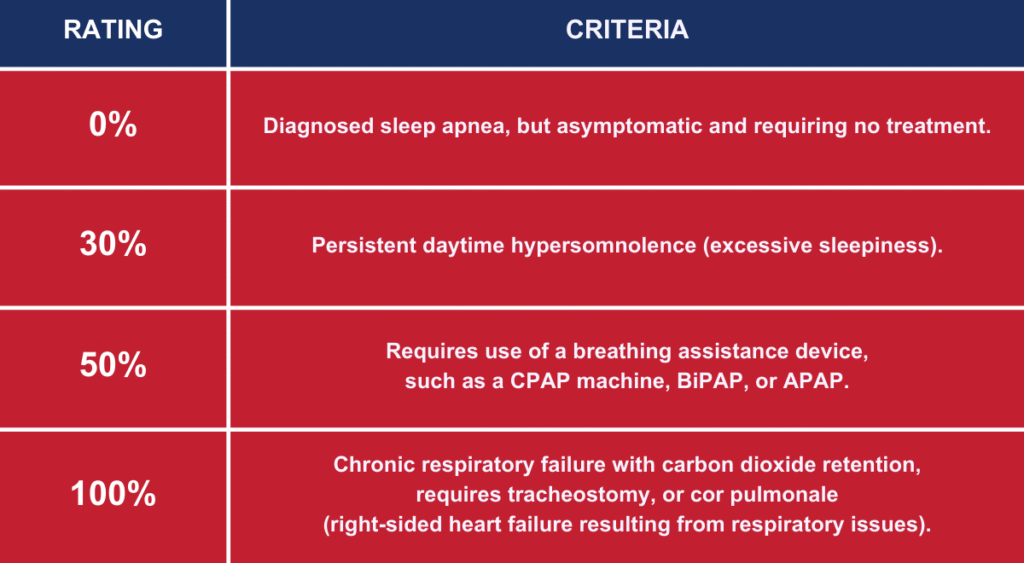
The 50% rating assigned for needing a prescribed treatment like a CPAP machine is a significant element, particularly concerning the proposed changes. This current “automatic” 50% rating for CPAP prescription use is the focus of much discussion. You can find the official language in the Electronic Code of Federal Regulations.
Why is the VA Thinking About Changing Things?
The VA periodically reviews and updates the VA Schedule for Rating Disabilities (VASRD). The stated purpose of these reviews is to ensure the disability ratings accurately reflect current medical understanding of diseases and injuries. They also aim to ensure the rating criteria provide fair compensation based on average earnings loss.
Officials have indicated a desire for rating criteria based more on the actual functional impairment caused by a condition. This approach focuses on how the disability impacts a veteran’s ability to work and function daily. It moves away from relying solely on the type of treatment needed.
Regarding sleep apnea, the perspective seems to be that prescribed treatment, specifically CPAP therapy, is often an effective treatment. The reasoning follows that if a CPAP machine successfully controls apnea symptoms, the individual might not experience significant occupational or social impairment. Therefore, a high rating based only on needing the device might not reflect the actual level of disability experienced if treatment effectiveness is high.
These comprehensive reviews aim to modernize criteria across numerous health conditions, not just sleep apnea. Proposed rule changes are typically published in the Federal Register, allowing for public comment before final decisions are made. This process allows stakeholders, including veterans and advocacy groups like VA Claims Insider, to provide input.
Understanding Upcoming Changes in VA Sleep Apnea Rating Criteria: The Proposals
This is where the details become important, but keep in mind: these are proposed VA sleep apnea rating changes, and nothing is finalized. The VA introduced these proposals back in February 2022, but they have not yet been implemented.
The most substantial suggested alteration impacts the 50% sleep apnea rating. Under the proposal, requiring a CPAP machine would no longer automatically qualify a veteran for a 50% rating. This marks a potential major shift in how VA sleep apnea is evaluated.
Instead, the proposed apnea rating criteria would likely base the disability rating more on the severity of residual sleep apnea symptoms after treatment. It would also consider situations where treatment is ineffective or not feasible for the veteran. The focus shifts from treatment device necessity to treatment outcome and remaining impairment.
Moving Away from CPAP as the Main Factor
The proposal suggests that if a CPAP machine or another breathing device successfully manages the condition and controls apnea symptoms, the rating could be significantly lower. It might be 10% or even 0%, even though the veteran still requires the device nightly.
This change reflects the idea that effective treatment mitigates the disabling effects of the condition. If symptoms are resolved, the functional impairment is lessened, according to this view. This is a stark contrast to the current system where CPAP prescription alone triggers the 50% level.
This specific proposed change is the primary source of concern for many veterans. Those currently holding a 50% current rating based solely on CPAP use worry about potential future reductions if re-evaluated under new rules. Brian Reese of VA Claims Insider often discusses the implications of these potential shifts.

Focus on Lingering Symptoms and Treatment Failure
Under the proposed rules, achieving a higher rating would likely require demonstrating that sleep apnea symptoms persist despite consistent treatment. This could involve proving ongoing issues like persistent daytime sleepiness, cognitive difficulties, or fatigue even with compliant CPAP use. A sleep study showing ineffective treatment might become crucial evidence.
Higher disability ratings could also be assigned if prescribed treatments are ineffective or if significant complications arise from sleep apnea. Examples include the development of comorbid conditions like pulmonary hypertension or evidence of end-organ damage such as cardiovascular disease linked directly to the poorly controlled sleep apnea. Documentation showing ineffective treatment would be essential.
The evaluation emphasis moves towards the actual, persistent disability that impacts a veteran’s daily life, work capacity, and overall health. Documented organ damage related to sleep apnea would likely support a higher rating. Proof that treatment is not effective treatment would be necessary.
Possibility of Lower Ratings for Some
It is accurate that under the proposed changes, some veterans might receive lower disability ratings for sleep apnea compared to the current criteria. If a veteran has sleep apnea, uses a CPAP machine, and the treatment effectively eliminates all symptoms, their rating might be assessed at 10% or 0% if evaluated under the new rules for the first time.
This potential for reduced compensation understandably worries many veterans currently navigating the VA claims process or those already receiving benefits. It underscores the importance of understanding the current system and the potential impact of future changes. This is why discussions led by experts like Brian Reese Brian Reese gain attention.
However, it’s critical to reiterate that these changes are not yet active. Furthermore, established VA disability ratings generally have protections against arbitrary reductions, especially those based purely on changes in rating schedules.
The Big Question: When Will This Happen?
This remains the most significant uncertainty, and there is no definitive timeline. The VA proposed these rating criteria changes back in February 2022.
Altering the VA rating schedule is a lengthy, multi-step administrative process. It involves publishing proposed rules, gathering and analyzing public comments, potentially revising the proposal based on feedback, and finally issuing a final rule with an effective date. There is often a 60 day implementation window or longer after the final rule is published.
This entire sequence can take several years to complete. It’s also possible that proposed rules are withdrawn or significantly modified before becoming final regulations. Currently, the VA has NOT announced any specific implementation date for the proposed sleep apnea rating changes for the upcoming calendar year or beyond.
Looking at past updates to the VASRD for other conditions provides context. Some updates have taken many years to move from the proposal stage to final implementation. While the wait and uncertainty can be frustrating for veterans, patience is often required during these regulatory review periods.
What About Veterans Already Rated for Sleep Apnea?
This is a crucial point that generates significant anxiety among current claimants receiving disability benefits. What happens if you already possess a 50% VA sleep apnea rating based on your CPAP prescription under the current rules?
Generally, the VA has regulations designed to protect established disability ratings from being easily reduced. This concept is sometimes referred to as “grandfathering,” although the VA employs terms like “stabilized rating,” “continuous rating,” or “protected rating.” Specific rules govern when and how a rating can be lowered.
Ratings that have been in effect for extended periods (5, 10, or 20 years) acquire increasing levels of protection against reduction, as detailed in VA regulations such as 38 CFR § 3.951 (Preservation of disability ratings) and § 3.957 (Combined ratings). Importantly, the VA typically cannot reduce a veteran’s established rating solely because the rating schedule itself has changed. The criteria based on the time of the original decision usually apply unless specific conditions for re-evaluation are met.
A rating reduction usually necessitates medical evidence demonstrating that the veteran’s actual medical condition has materially improved on a sustained basis under ordinary conditions of life (excluding periods of hospitalization or convalescence). Therefore, if you are already service-connected and rated for sleep apnea, your current rating is likely protected from the proposed changes, assuming your underlying sleep apnea condition has not genuinely improved. This protection applies even if the rules change for new VA disability claims filed after the implementation date.
Why Filing Your VA Claim Now is So Important
Given that the current, potentially more favorable rules are still active and future changes remain uncertain, filing your sleep apnea claim now is a prudent strategy. If you suspect your sleep apnea is linked to your military service, initiating the VA claim process sooner rather than later is highly recommended.
Submitting your disability claim under the current rating criteria means the VA will evaluate it based on the rules in effect today. If your claim is granted, establishing service connection and receiving a rating (such as the 50% for CPAP use), that rating will likely gain the protections discussed earlier against future schedule changes.
Waiting until new, potentially stricter rules are implemented could make obtaining a higher rating more challenging, especially if the requirement shifts from CPAP use to proving ineffective treatment or significant residual symptoms. Acting now effectively locks in your evaluation under the existing, known system. Don’t delay gathering your medical evidence and submitting your application.
Getting Service Connection for Sleep Apnea
To receive VA disability benefits for sleep apnea, proving service connection is essential. This involves demonstrating a clear link or nexus between your current sleep apnea diagnosis and an event, injury, or disease that occurred during your military service.
There are several pathways to establish this connection. You fundamentally need three things: a current medical diagnosis of sleep apnea (confirmed by a sleep study), evidence of an in-service incident, injury, exposure, or illness, and a medical opinion connecting the first two elements (often called a nexus letter).
Gathering comprehensive and relevant evidence is crucial for strengthening your disability claim and increasing the chances of a favorable outcome. Missing documentation or weak linkage evidence can lead to delays or denials of VA benefits.
Direct Service Connection
This is the most straightforward path. It applies if your sleep apnea symptoms began or were diagnosed while you were still on active duty. Evidence might include notations of snoring, excessive daytime sleepiness, breathing problems, or related complaints in your Service Treatment Records (STRs).
Even if the formal diagnosis occurred after separating from service, you could still argue for direct service connection if you can show symptoms started during service. Supporting statements from fellow service members who witnessed your symptoms (buddy statements) can be valuable here.
Secondary Service Connection
This is an extremely common route for sleep apnea claims. Here, you argue that your sleep apnea was caused or aggravated by another condition for which you are already service-connected. This acknowledges that many health conditions are interrelated.
Frequent conditions linked secondarily to sleep apnea include PTSD, chronic sinusitis or rhinitis (due to airway obstruction), asthma, TBI, medication side effects (from drugs treating other service-connected issues), or weight gain resulting from reduced mobility due to a service-connected injury (like back, knee, or hip problems). For these claims, you absolutely need strong medical evidence, often a nexus letter from a doctor, clearly explaining the physiological link between the primary service-connected condition and the development or worsening of sleep apnea. For example, inflammation from sinusitis can narrow nasal passages, contributing to OSA, or PTSD-related hyperarousal might affect sleep architecture.
Research studies demonstrating statistical links, like the strong association between PTSD and sleep apnea, can further support these secondary claims. Establishing this link clearly through medical opinion is key for these types of disability claims.

Aggravation
If you had a diagnosis of sleep apnea before joining the military, you might still get service connection through aggravation. This requires showing that your military service permanently worsened the pre-existing condition beyond its natural progression. This means proving your service made the apnea symptoms substantially worse than they would have become otherwise.
Proving aggravation typically requires detailed medical records from before service to establish a baseline severity, evidence from service showing worsening, and post-service records demonstrating the increased level of disability. A medical opinion confirming that the worsening was due to service factors and not just natural progression is usually necessary. This path can be more complex and requires meticulous documentation.
What Evidence Do You Need to File?
A well-supported VA claim requires thorough and organized evidence. Insufficient documentation is a common reason why disability claims get denied or delayed during the VA claims process.
Key pieces of evidence generally needed for a sleep apnea claim include:
- Your DD-214 or other separation documents verifying your service details.
- Service Treatment Records (STRs): Look for any entries mentioning snoring, daytime fatigue, difficulty sleeping, breathing issues, referrals to sleep clinics, or treatment for related conditions like PTSD, sinus problems, or relevant injuries.
- Current Medical Records: These must confirm your current diagnosis of sleep apnea. Crucially, this MUST include the official report from a diagnostic sleep study (polysomnogram or home sleep test).
- Proof of Prescribed Treatment: Documentation showing you have been prescribed a breathing device like a CPAP machine. This could be the CPAP prescription itself, records from the DME supplier, or CPAP usage/compliance data if available.
- Medical Nexus Letter: This is often the most critical piece of evidence, especially for secondary claims or claims filed long after service. It’s a statement from a qualified medical professional reviewing your records and providing a reasoned opinion linking your sleep apnea directly to your service (e.g., in-service event, injury) or secondarily to another service-connected condition. The letter should explain the rationale for the connection using medical literature or principles if possible.
- Lay Evidence / Buddy Statements: Written statements from you (VA Form 21-4138, Statement in Support of Claim), your spouse, family members, friends, or fellow veterans describing your sleep apnea symptoms, when they began, how they impact your daily life, and any observed connection to your service or other conditions. These personal accounts can help fill gaps in official records.
Carefully compiling and submitting this medical evidence with your VA Form 21-526EZ (Application for Disability Compensation and Related Compensation Benefits) will significantly strengthen your VA disability claim. Being thorough helps the VA rater understand the full picture of your condition and its connection to service.
Conclusion
The situation regarding potential changes to the VA sleep apnea rating criteria is ongoing and not yet finalized. While understanding upcoming changes in VA sleep apnea rating criteria is valuable for awareness, the primary points for veterans remain consistent.
Proposed modifications, particularly regarding the 50% rating for CPAP use, are currently just proposals. They are not final rules and lack a confirmed implementation date or day implementation window. Veterans currently receiving VA disability benefits for sleep apnea generally have protections (stabilized ratings) against reductions based solely on changes to the rating schedule; improvement in the actual condition must typically be shown.
The most beneficial action veterans can take right now is to file their sleep apnea claim without delay if they believe the condition is connected to their military service. Filing now ensures the VA claim will be evaluated under the current, known apnea rating criteria. This potentially secures disability benefits, including a possible higher rating, before any future, potentially less advantageous rules might take effect for new disability claims.


